RECOMMENDATIONS FOR PREVENTION OF POSTPARTUM HEMORRHAGE: FIGO GUIDELINES 2022
•• The use of uterotonics for prevention of PPH during the third stage of labor is recommended for all births. Oxytocin (10 IU intravenously/intramuscularly [IV/IM]) is recommended for the prevention of PPH for vaginal delivery and cesarean section. In settings where oxytocin is used, attention should be paid to the oxytocin cold chain.
•• In settings where oxytocin is unavailable or its quality cannot be guaranteed, the use of other injectable uterotonics (if appropriate ergometrine/methylergometrine 200 μg IM/IV; hypertensive disorders can be safely excluded prior to its use) or oral misoprostol (400–600 µg orally) or carbetocin 100 µg IM/IV is recommended for the prevention of PPH.
•• The combinations of ergometrine plus oxytocin or misoprostol plus oxytocin may be more effective uterotonic drug strategies for the prevention of PPH ≥500 ml compared with the current standard, oxytocin. This comes at the expense of a higher risk of adverse effects (vomiting and hypertension with ergometrine and fever with misoprostol).
•• In settings where skilled birth attendants are not present to administer injectable uterotonics and oxytocin is unavailable, the administration of misoprostol (400–600 μg orally) by community healthcare workers and lay health workers is recommended for the prevention of PPH.
•• In settings where skilled birth attendants are unavailable, controlled cord traction (CCT) is not recommended.
Sustained uterine massage is not recommended as an intervention to prevent PPH in women who have received prophylactic oxytocin.
•• Postpartum abdominal uterine tonus
assessment for early identification of uterine atony is recommended for all women.
•• Oxytocin (IV or IM) and CCT is the recommended method for removal of the placenta for the prevention of PPH in cesarean delivery.
RECOMMENDATIONS FOR TREATMENT OF POSTPARTUM HEMORRHAGE:
•• Intravenous oxytocin alone is the recommended first-line uterotonic drug for the treatment of PPH.
•• If intravenous oxytocin is unavailable, or if the bleeding does not respond to oxytocin, the use of intramuscular ergometrine, oxytocin–ergometrine fixed-dose, or a prostaglandin drug (including sublingual misoprostol, 800 μg) is recommended.
•• There is no evidence about the safety and efficacy of an additional 800-μg dose of misoprostol for treatment of PPH when given to women who have already received 600 μg of prophylactic misoprostol orally.
•• The use of isotonic crystalloids is recommended in preference to the use of colloids for the initial intravenous fluid resuscitation of women with PPH.
•• Basic recommendations for resuscitation in PPH include administration of crystalloids in small boluses of 500 ml, checking clinical signs and looking for its improvement, and use of balanced crystalloid solutions such as Ringer’s lactate, which is preferred over chlorine-rich solutions. The target blood pressure in hypotensive resuscitation is 80–90 mm Hg for systolic blood pressure or 50–60 mm Hg for mean blood pressure.
•• In hemostatic reanimation, fewer crystalloids are administered and, instead, transfusional replacement is started earlier with high ratios of transfusion (1:1:1). During massive transfusions, the target for serum fibrinogen is 150–200 mg/dl and the usual dose of cryoprecipitate is 10 units; it is estimated that these will raise the serum fibrinogen by 100 mg/dl. The protocol for massive transfusion is specific at Each institution. Physicians should be familiar with their hospitals’ protocol and recommendations.
Massive transfusion protocol in obstetrics:
•• Early use of intravenous tranexamic acid as soon as PPH is diagnosed but within 3 h of birth in addition to standard care is recommended for women with clinically diagnosed PPH following vaginal birth or cesarean delivery.
•• Administration of 1 g (100 mg/ml) tranexamic acid intravenously at 1 ml/min (i.e. administered over 10 min), with a second dose of 1 g intravenously if bleeding continues after 30 min, or if bleeding restarts within 24 h of completing the first dose. Reducing maternal deaths due to bleeding through scaling up of tranexamic acid for PPH treatment could have a positive impact on health equity and improve outcomes among disadvantaged women, especially in LMICs.
•• Uterine massage is recommended for the treatment of PPH.
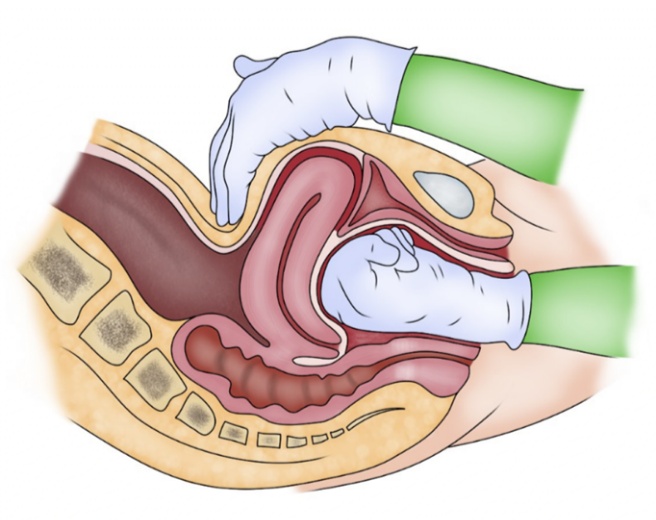
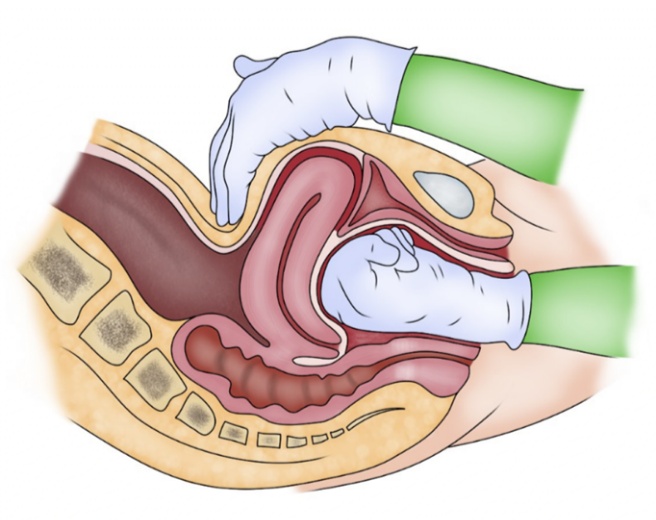
•• The use of bimanual uterine compression or external aortic compression for the treatment of PPH due to uterine atony after vaginal birth is recommended as a temporizing measure until appropriate care is available.
•• If women do not respond to treatment using uterotonics, or if uterotonics are unavailable, the use of uterine balloon tamponade is recommended as an effective non-surgical technique that can potentially improve survival in women with PPH due to uterine atony after ruling out retained products of conception or uterine rupture as a contributing factor.
•• Use of the nonpneumatic antishock garment (NASG) is recommended as a temporizing measure until appropriate care is available. NASG is an effective non-surgical device that can help to recover hemodynamic stability for the management and transfer of a patient to a high level of care.
•• The use of uterine packing is not recommended for the treatment of PPH due to uterine atony after vaginal birth.
•• Uterine artery embolization can be another conservative management measure for PPH if technical conditions and skilled human resources are available for its use.
•• If bleeding does not stop despite treatment using uterotonics and other available conservative interventions (e.g. uterine massage, balloon tamponade), the use of surgical interventions is recommended. Surgical interventions include the use of compression suture techniques, uterine and hypogastric artery ligation, and hysterectomy.
•• The priority is to stop the bleeding before the patient develops coagulation problems and organ damage from under-perfusion. Conservative approaches should be tried first, rapidly moving to more invasive procedures if these do not work.
•• Damage control resuscitation (DCS) is a combination of resuscitation and surgical interventions with the purpose of restoring hemostasis and normal physiology. These techniques have proven to be applicable in obstetrics, with satisfactory results controlling refractory PPH and an overall decreased mortality of critically ill patients, especially in patients in whom conventional treatment can be linked to a high risk of failure. DCS is an available therapeutic approach for the management of severe PPH, thus proper training must be widespread to implement this technique.
Administration of TXA:
•• Administration of TXA is recommended as soon as the diagnosis of PPH is made if the diagnosis is made within 3 h of delivery. When more than 3 h has elapsed since delivery, there is no clear evidence of benefit from TXA administration.
•• TXA, as a management strategy, in addition to uterotonics reduced the risk of PPH in randomized trials. Usually, 1 g TXA intravenously is recommended within 10 min after vaginal delivery in addition to oxytocin, cord traction, and uterine massage.
•• TXA should be given to all women with clinically estimated blood loss of more than 500 ml after vaginal birth or 1000 ml after cesarean delivery, or any blood loss that is sufficient to compromise hemodynamic stability, regardless of the cause of hemorrhage.
Reference : FIGO recommendations on the management of postpartum hemorrhage 2022
AU: Maria Fernanda Escobar, Anwar H. Nassar, Gerhard Theron, Eythan R. Barnea, Wanda Nicholson, Diana Ramasauskaite, Isabel Lloyd, Edwin Chandraharan, Suellen Miller, Thomas Burke, Gabriel Ossanan, Javier Andres Carvajal, Isabella Ramos, Maria Antonia Hincapie, Sara Loaiza, Daniela Nasner, FIGO Safe Motherhood and Newborn Health Committee