1 – VTE in Bone Metastasis
- A. What is the overall risk for VTE in this patient population and what are the factors that increase VTE risk in this patient population?
- B. What is the optimal VTE prophylaxis protocol in this patient population when also taking into consideration bleeding risk?
Response/Recommendation: Patients that undergo prophylactic fixation or pathological fracture fixation due to metastatic bone disease have a high risk of developing venous thromboembolism (VTE). Risk factors include patient characteristics such as age and comorbidities, as well as extent of surgery and duration of surgery. In the absence of contraindications, patients that undergo surgery or hospitalized patients should be administered thromboprophylaxis with or without mechanical prophylaxis. At this time, we do not have sufficient evidence to make specific recommendations for the type of thromboprophylaxis.
A. What is the overall risk for VTE in this patient population and what are the factors that increase VTE risk in this patient population?
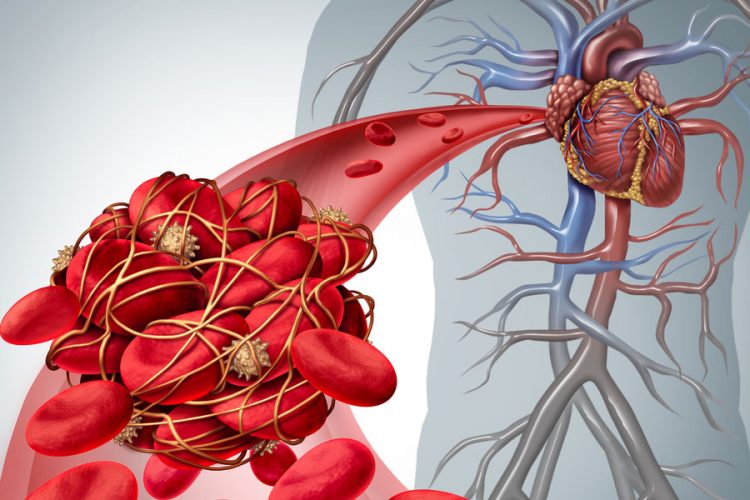
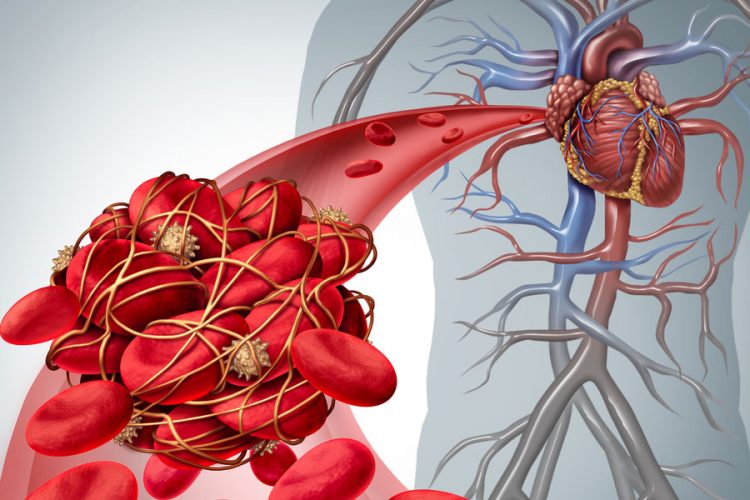
Rationale: VTE, encompassing deep venous thrombosis (DVT) and pulmonary embolism (PE), is a major public health problem that affects 300,000 to 600,000 individuals in the United States each year and is accompanied by considerable morbidity and mortality. Some of that is related to bone tumors and bone metastasis.
Patients with long-bone or spinal metastases who undergo surgery have a high risk of developing VTE, with VTE diagnosed in 6% following long bone surgery and with an overall incidence of VTE in spinal surgery (16.9%). The average age for patients with VTE in spine metastasis surgery was 57 years and 62% were male. Risk factors also include type of operation. One study noticed that it is highly unlikely for patients with intramedullary nails to develop DVT compared to patients with knee prostheses (odds ratio [OR] = 0.11, relative risk [RR] = 1.16). Patients that underwent prophylactic fixation had a significantly higher rate of PE than the pathological fracture group (2.1% compared with 1.2%; p = 0.008), with an OR of approximately 2.0.
Blood transfusions are known to increase the risk of VTE events in overall cancer patients. Khorana et al., found VTE rates of 7.2% (venous) and 5.2% (arterial) in cancer patients that received red blood cell transfusions. These rates were significantly higher than the comparative group that did not receive a transfusion. (3.8 and 3.1%). Therefore, a cautious approach to the use of blood transfusions during metastatic bone cancer surgery is recommended.
Some studies have explored the association between operative time and postoperative VTE. Tominaga et al., found that 20 of 80 patients had VTE after spinal surgery. The median operative time for patients with VTE and without VTE was 212.5 minutes and 177.5 minutes, respectively. A large-scale retrospective study in spinal metastatic patients showed that longer operative time was independently associated with an increased risk of postoperative symptomatic VTE. The risk of VTE increased by 15% for every additional hour of surgery. Operative time of ≥ 4 hours was an independent predictor of VTE after spinal surgery.
Patients who undergo surgical treatment for lower limb pathological fracture due to malignancy are at increased risk of DVT or death due to PE under current general thromboprophylaxis regimens. The risk is higher for the immediate postoperative period (10 days). The risk is increased by the presence of other metastases, arthroplasty reconstruction, and perioperative adjuvant therapy (radiotherapy, chemotherapy).
B. What is the optimal VTE prophylaxis protocol in this patient population when also taking into consideration bleeding risk?
Rationale: Previous studies have shown that the rate of VTE in patients receiving VTE prophylaxis was 9.1% in the group that received early prophylaxis (days 1–3) and 35.7% in the delayed group (26.6% absolute risk reduction; p=0.049). Patients who underwent prophylactic fixation of a metastatic femoral lesion had a significantly higher rate of PE than the pathological fracture group (2.1% compared with 1.2%; p = 0.008), with an OR of approximately 2.0. There was no difference in VTE events between the type of anticoagulation used. (OR = 0.21, RR = 0.98).
There is limited literature on what the optimal prophylaxis for orthopedic oncology and metastasis surgery. The guideline for treatment for cancer patients in general stated by the American Society of Clinical Oncology (ASCO) is divided on patient categories, such as: hospitalized patients, outpatients, patients undergoing surgery, and patients with established VTE. In hospitalized patients who have active malignancy and acute medical illness or reduced mobility, pharmacologic thromboprophylaxis should be offered in the absence of bleeding or other contraindications but should not be offered for the sole purpose of minor procedures or chemotherapy infusion. Not all cancer outpatients require VTE prophylaxis, and the decision to use prophylaxis depends on the type of cancer being treated and the type of chemotherapeutic regimen.
All patients with malignant disease undergoing major surgical intervention should be offered pharmacologic thromboprophylaxis unless contraindicated due to active bleeding, or high bleeding risk, or other contraindications. Thromboprophylaxis is initiated preoperatively. Mechanical prophylaxis should not be the only precautionary method used and should be combined with pharmacological thromboprophylaxis in high risk patients.
Regarding the choice of VTE prophylaxis, different kinds of agents including low-molecular-weight heparin (LMWH), Vitamin K Antagonist (VKA), Direct Oral Anti Coagulants (DOAC) and also aspirin are appropriate. One study reported that aspirin significantly lowered the incidence of acute PE, but the risk of major bleeding is the same between two groups.
A network meta-analysis reported that the OR for recurrent VTE in the group receiving VKA was 0.67 (95% confidence interval [CI], 0.40-1.15, p 0.147), and 0.96 (95% CI, 0.52-1.75, p 0.886) in the group LMWH. Anticoagulants such as LMWH emerged with the highest cumulative ranking probability for the efficacy endpoint, while DOAC had the highest cumulative ranking probability for the safety endpoint. Other studies reported that DOAC lowered the incidence of 6-month recurrent VTE when compared to LMWH (RR 0.56, 95% CI 0.40–0.79; p < 0.001, estimated heterogeneity [I] 59%) and incidence of major bleeding was not significantly different between DOAC and LMWH treated patients (RR 1.56, 95% CI 0.95–2.47, p = n.s.). However, another meta-analysis showed that LMWH has significant reduction in recurrent VTE events (RR: 0.52; 95% CI: 0.36 to 0.74) whereas DOAC did not (RR: 0.66; 95% CI: 0.39 to 1.11).
LMWH has shown efficacy and safety comparable with the use of DOAC in patients with cancer and VTE, with a non-significant trend toward a better efficacy with DOAC while LMWH was associated with lower rates of bleeding over DOAC. We conclude that larger studies regarding optimal VTE prophylaxis are required to make definitive conclusions as to the most efficacious and safe thromboprophylaxis in bone metastasis patients.
References: